A POLITICAL PERSPECTIVE ON LONG COVID
At Winslow, we have been eager to explain our vision of Long COVID for a long time. Since the start of the COVID-19 epidemic in 2020, almost every national and international institution, from the World Health Organization (WHO) to the French High Authority for Health (HAS, Haute Autorité de Santé), has made its own contribution to recognizing and defining the disease that affects the majority of our members. Other public health institutions, however, did not seem to be in any hurry to recognize us as patients: we had to wait until November 7, 2023, for the Committee for Monitoring and Anticipating Health Risks (COVARS, Comité de veille et d’anticipation des risques sanitaires), an organization supposed to be at the forefront of monitoring and anticipating health risks in France, to give us its opinion on Long COVID. Better late than never, right?
In any case, from one institution to another, what remains unchanged is that patients have often been used as leverage in the process of official recognition of their own illness, without this translating into care that is truly adapted to their ordeal. Long live healthcare democracy! Yet, as people living with Long COVID, aren’t we in the best position to provide an accurate and comprehensive representation of what Long COVID is?
Especially since, regardless of what public health institutions may say in hindsight, the conceptualization of Long COVID and its implications did not originate with them. It was expert patients who had survived the acute infectious phase of COVID-19 and were experiencing firsthand what it was like to live with the SARS-CoV-2 virus for an indefinite period of time who, in early 2020, coined the term “Long COVID” (notably thanks to Elisa Perego, Elisa Perego, an expert patient and researcher). It was the patients who laid the groundwork for understanding this new chronic disease, compensating for the usual slowness and inaction of governments when it comes to protecting the population from a major risk. From climate change to COVID-19 to the HIV/AIDS epidemic, it is almost always the same story that repeats itself.
As an association of people living with Long COVID and people with disabilities and/or chronic illnesses who have been severely affected by the COVID-19 epidemic, we are continuing this effort to empower those affected to take ownership of their illness. Nothing about us without us.
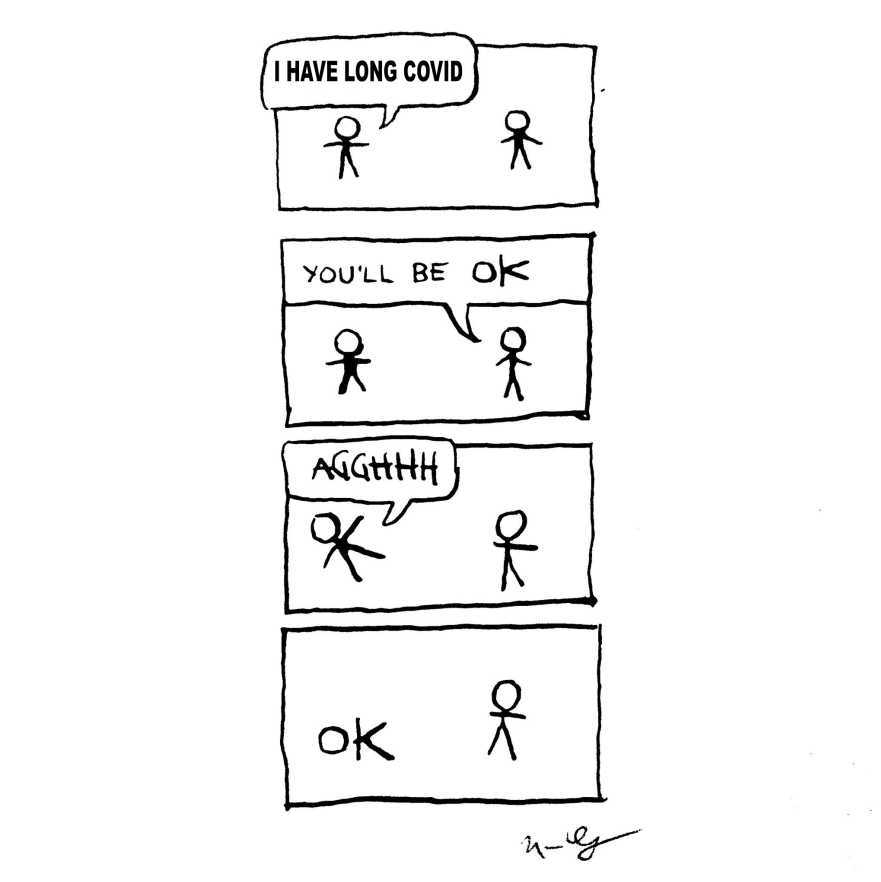
1- LOOOOOONG COVID
In October 2021, the WHO suggested the term “Post-COVID Condition” to encompass people with a history of probable or confirmed SARS-CoV-2 infection, generally 3 months after the onset of COVID-19, with symptoms that persist for at least 2 months and that cannot be explained by another diagnosis. These symptoms can fluctuate or reoccur over time and generally have an impact on daily life. In France, the HAS (French National Authority for Health) congratulated itself on having expanded this definition by lowering the duration required to be able to use the term “Post-COVID Syndrome”: if symptoms persist beyond four weeks after the acute phase, patients are diagnosed with the condition.
It seems like the term “Long COVID” didn’t really suit the institutions. Instead of a straight-forward term that reflects the chronic nature of COVID-19 experienced by many infected people (Loooong COVID), institutions prefer a term that sounds like an attempt to artificially create a discontinuity in people’s mind between the acute phase of the disease (COVID-19) and the chronic phase (post-COVID, i.e., literally, the after COVID). By focusing solely on Long COVID symptoms, who only make sense in relation to each other and because they are the result of an infection with the virus that causes COVID-19 and specific pathophysiological mechanisms, institutions officially integrate the disease in the ‘post-acute infection syndromes’ (PAIs) category. Defined as sets of symptoms that persist after the acute phase of a viral or bacterial infection, PAIs appear to be a long list of chronic diseases that have been concealed and glossed over for decades by healthcare professionals and governments who seem in no hurry to understand and treat their specific causes and mechanisms. This would indeed require them to dedicate sufficient resources to the understanding and treatment of each PAI. In other words, it would cost a lot more. In order to continue doing nothing, might as well stick the same catch-all label on people infected with pathogens as different as influenza, Ebola, or dengue, on the basis of certain very generic common symptoms, who would merely be the remnants of a now over infection. It’s as if it would be inconceivable that a chronic disease of infectious origin could persist well beyond the infection’s acute phase and evolve, disable or even kill in the long term. Yet, from papillomaviruses to HIV, viral hepatitis, EBV or syphilis, it is very clear that many viruses and bacteria cause chronic infections and debilitating or fatal diseases (cancers, auto-immune diseases such as multiple sclerosis, dysimmunity…) even several years after the initial infection. It is of the utmost urgency to apply a similar paradigm to people infected with SARS-COV-2.
2- LONG COVID IS NOT JUST ABOUT THE SYMPTOMS
In France, doctors diagnose Long COVID basing themselves on a clinical picture consisting of “more than 200 symptoms” and by ruling out other possible diagnoses that could explain the symptoms. This approach does not allow for a proper identification of all the people affected, nor does it allow for an objective assessment of the severity of their condition. Should we remind the doctors that a condition known as pathological, resulting from the presence of one or more pathogens (which is called a disease in everyday language), has manifestations that can be directly seen or experienced by the patient (clinical symptoms), but also more subtle ones, that are not directly visible or felt — or not as abnormalities. In this case, there are still manifestations and characteristic signs, but only accessible through microscopic observations, biochemical tests, and molecular biology analyses. Cancer, for instance, can be completely asymptomatic (in the sense that the patient doesn’t experience anything unusual, and there are no visible clinical signs) before the damage it causes triggers recognizable clinical signs. The same is true for contagious diseases. In other words, the absence of clear, visible symptoms (clinical signs or the patient’s experience) does not mean that a disease does not exist or is not there. Similarly, clinical symptoms of a disease can differ from one patient to another, even if the cause (etiology) is the same. Conversely, a set of identical symptoms can stem from different causes in different patients.
According to current scientific knowledge, SARS-COV-2 can affect every organ in the human body, which explains the large variety of symptoms observed in people with Long COVID. However, not all damage caused by the virus in the human body is necessarily directly visible or felt by patients. Debilitating or fatal manifestations of Long COVID can also occur weeks or even months after infection, including in the form of diseases that exist independently from Long COVID (e.g., lupus or antiphospholipid antibody syndrome which, when triggered by SARS-COV-2, do fall within the Long COVID spectrum). The manifestations of the disease can also evolve and worsen. Symptoms alone also do not necessarily indicate Long COVID and provide only a partial picture, insufficient in order to properly care for patients. Long COVID symptoms can also manifest or be experienced differently depending on whether you are a child, a young adult, a woman, a person who is already disabled and chronically ill, a person of color, an elderly person… We also know that, as it is the case with many viruses, the acute phase of COVID-19 can often be asymptomatic (i.e., without any visible symptoms that would prompt the infected person to seek testing at the time of infection) and yet still lead to a form of Long COVID with disabling and potentially fatal consequences. Without the infected person being aware of having been recently (re)infected, and given the level of denial among doctors on the current health crisis, (“COVID-19 is over” is maybe one of the sentences chronically ill people hear the most when they go to a healthcare facility wearing a mask), it is extremely unlikely that a doctor will think of Long COVID based on a list of generic symptoms.
Diagnosing Long COVID based solely on symptoms further exacerbates the imbalance in the doctor/patient relationship, at the expense of patients. Not all doctors, but many nonetheless, validate or invalidate our experiences on a whim, diagnosing the presence or absence of Long COVID by shooting from the hip, without even performing the proper tests and examinations (the existence of which they often learn about from expert patients). Few update their knowledge as scientific research progresses, and even fewer are those who actively deconstruct their sexist, racist, ableist, classist biases, which lead them to arbitrarily include or exclude a person from a Long COVID diagnosis and its specific treatments.
3- LONG COVID IS COVID
It is therefore necessary to hammer home again and again that Long COVID is COVID. Or more precisely, that the SARS-CoV-2 virus is responsible for a disease in humans, COVID, and that this disease ranges from an acute phase lasting an average of ten days to a chronic phase that is very (too) common. For the first people affected by Long COVID, this chronic phase has now lasted for more than five years, despite the efforts of various quacks who still insist on psychologizing patients and explaining Long COVID by referring to “personality” or “behavior” (they clearly don’t care much about scientifically rigorous approach). Because the real problem is the pathogen. So let’s call the chronic phase of Long COVID, chronic COVID, or persistent COVID, but certainly not “Post-COVID Syndrome.” Especially when we know that for a large proportion of people living with Long COVID, infection with the virus is probably still ongoing. And although Long COVID shares many symptoms in common with other systemic diseases, it differs fundamentally in its cause, which justifies specific funding, research, and clinical trials, as should be the case for every systemic disease.
The main criterion for belonging to the Long COVID category remains the experience of infection with the COVID-19 virus, which should be documented during the acute infectious phase but also during the chronic phase. There are measurable biological signs of chronic infection with the COVID-19 virus, but also other mechanisms of the disease (thromboinflammation, dysimmunity, etc.). In serious research protocols, objective tests and markers are therefore increasingly being used to recruit Long COVID patients. So why are these tests not available to the general public? Who would not want to know if they have a chronic COVID-19 virus infection, or markers linked to other Long COVID mechanisms, even in the absence of very debilitating symptoms at a given moment? This Long COVID screening would also allow people who have been infected with the COVID-19 virus at least once in their lives (i.e., almost everyone in France) to make the connection with any illnesses that may have been triggered since the start of the COVID-19 epidemic, illnesses that may be caused or aggravated by the COVID-19 virus and therefore fall squarely within the spectrum of Long COVID. These include autoimmune, neurological diseases, heart and lung diseases, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), diabetes, digestive diseases, EDS, blood clots, strokes, etc.
But we know that it has become particularly difficult to know when we have been reinfected with the COVID-19 virus now that epidemiological monitoring has been carefully dismantled by the health authorities, in particular the French Directorate General for Health (DGS, Direction Générale de la Santé). The SI-DEP system has been abandoned, PCR tests are no longer reimbursed, and prevention campaigns are anecdotal given the scale of the epidemic, giving rise to an infodemic by conflating, for example, the COVID-19 virus, which circulates all year round, with winter viruses such as the common cold or flu… In June 2020, Donald Trump explained that “If we stopped testing now, we would have very few cases, if any.” Donald Trump dreamed of it, France did it. No testing, no COVID. No COVID, no Long COVID. It is even more grotesque when we remember that COVID-19 is supposed to be a notifiable disease. Ultimately, who will still be able to access a diagnosis of Long COVID in the years to come? With the invisibility of the virus circulation and the lack of specific training for healthcare professionals on the subject, the term “Long COVID” is being used less and less. People are disabled and dying from a disease that no longer has a name.
Increasingly, people are also being removed from the Long COVID category (and its specific treatment) when another disease is diagnosed that appears to explain certain symptoms, even though this disease is often one of the manifestations of Long COVID. The French government website sante.fr states the following:
For each persistent symptom reported by a patient, the doctor will seek to rule out other possible causes, starting with the most serious, so as not to overlook a disease other than Long COVID (e.g., pulmonary embolism, autoimmune disease, or cancer) or a serious consequence of the acute episode of COVID-19: this is the stage known as ‘differential diagnosis’”. However, as the NASEM points out in its définition of Long COVID, pulmonary embolisms and autoimmune diseases are an integral part of Long COVID when triggered by the COVID-19 virus.
4- LONG COVID IS NO LONGER A “MYSTERY”
By 2025, COVID-19 and its chronic form, Long COVID, are no longer “mysterious” and “misunderstood” as many doctors, journalists, and politicians still seem to believe. On the contrary, it is one of the most studied diseases in the history of medicine in such a short period of time, with tens of thousands of scientific studies having been published since the start of the pandemic in 2020.
We now know that COVID-19 is a systemic vascular disease, meaning it affects the blood vessels. Since blood vessels are found literally everywhere in the human body, Long COVID can show up in any organ: the heart, brain, lungs, digestive system, pancreas, and more. We also know the main mechanisms behind Long COVID:
- Viral persistence, which refers to the ability of SARS-CoV-2 to remain in the body for years after the acute phase of infection. Several recent studies have shown the presence of viral material in various tissues, even when the virus is no longer detectable in the upper respiratory tract or blood. This persistence may be explained by the forming of viral reservoirs, where the virus escapes the surveillance of the immune.
- Thromboinflammation: the development of microclots resistant to fibrinolysis is present in the majority of patients with Long COVID. These microclots block blood flow in small vessels, causing tissue damage, particularly to neurons and vital organs. They are responsible for symptoms such as chronic tissue hypoxia, cognitive impairment, etc. Furthermore, this mechanism can also complicate Long COVID by causing pulmonary thrombosis/embolism.
- Immune dysfunction: exhaustion and dysregulation of the immune system compromises the body’s ability to respond properly to infections (B cells depletion). In addition, a significant proportion of patients develop autoantibodies that target nerve and muscle tissue, leading to persistent symptoms. Long COVID can be a trigger for autoimmune diseases such as lupus, rheumatoid arthritis, and many others.
The main purpose of an official definition of Long COVID should therefore be to provide a summary of the scientific knowledge to date on the disease, enabling the number of patients to be accurately assessed and appropriate therapeutic and social care to be implemented. To fulfill its role, this definition must be regularly updated to remain continuously in line with the new knowledge that piles up every day, since it is truly the starting point for public health policy decisions and has repercussions on prevention, access to care, hospital budgets, training for healthcare professionals, and social rights (Medicaid, Medicare). So why is there no massive information and prevention campaign to help the population understand COVID-19 and its chronic form accurately? While the latest estimates worldwide show that the number of people affected by Long COVID is increasing significantly each year, reaching more than 400 millions in 2024,
making it one of the most common chronic diseases, in France we have not had any official census since 2022. In addition, some categories of patients, such as children, have been excluded from the census. In France, it is well known that children cannot catch COVID-19, so they cannot develop Long COVID. And according to prominent infectious disease specialists, people in “really severe” conditions represent only “10% of cases.” Source? Their best guess. The others are surely in a “mild” condition, such as the Omicron variant, and those who have died, have died of something else. A little “pacing” strategy, a few mindfulness meditation sessions, a spa treatment or two, and any damage to your brain, heart, or immune system is gone. Now you’re ready to go back to work and take care of your kids!
5- LONG COVID KILLS
On a more serious note, all current and future manifestations of Long COVID are serious and severe: strokes, pulmonary embolisms, ME/CFS, autoimmune diseases, dysimmunity and opportunistic infections, hypertension, dementia, etc. Losing a sense such as smell is not “mild.” Heart disease is neither easy to diagnose nor “well treated.” Post-Exertional Malaise (PEM) is not just “being a little tired.” “Brain fog” is brain damage or inflammatory fibrin. Blood clots are a significant risk factor for premature death, as are diabetes and hypertension. Of course, these various symptoms will handicap and endanger the person’s life to a greater or lesser degree, and must be treated appropriately. But it is crucial to stop ranking patients. On the one hand, because each of these symptoms can range from mild to severe, but also because, with only five years of hindsight, we cannot assess the severity of the disease solely on the basis of the level of disability. A disease that causes such organ damage and presents such risks of complications (remember that during the first year after infection, the risk of death from Long COVID is doubled) must also be assessed today in terms of life expectancy, as is the case for most chronic diseases. In addition, people living with Long COVID rarely have a single manifestation of the disease, but often several at the same time. Long COVID is also a progressive disease, both in terms of symptoms and organ damage, and it is impossible to say whether people who are currently “well” will not become severely disabled or die prematurely from an invisible Long COVID condition (e.g., cancer ?). This is especially true today, when even once a diagnosis has been made (if it is made at all), there is no follow-up or monitoring of these developments.
People die from COVID during the acute phase, but also during the chronic phase of the disease. It is crucial to continue to speak out about the fact that Long COVID kills.
And no one is immune to Long COVID. Healthy children develop Long COVID. Healthy young adults develop Long COVID. Athletes develop Long COVID. Defining Long COVID correctly also means moving away from attempts to pigeonhole disabled and chronically ill people into politically sterile categories such as “vulnerable” and “fragile,” categories used to reinforce their exclusion and the violence against them, while reassuring the “able-bodied” of their false immunity to disability and death. This does not prevent us from highlighting the fact that certain categories of people are at greater risk of certain manifestations of COVID-19 (direct death during the acute phase for immunocompromised people, for example), nor that certain political minorities are at greater risk of Long COVID due to discrimination in access to care and forced exposure to reinfection (women, people of color, people with disabilities and chronic illnesses, sex workers, LGBT people, prisoners, etc.). But vulnerability is a spectrum, and everyone is fragile and vulnerable to the COVID virus, especially after multiple reinfections, as the damage is cumulative. What doesn’t kill you comes back again and again until it does. Knowing this, and if we had the choice, who would consciously run the risk of reinfection by going to work, taking public transportation, or going to the hospital for treatment?
Without deliberately perpetuating a confused and erroneous view of the ongoing COVID-19 epidemic and its consequences, how would the state justify to the public the lack of prevention measures in hospitals, schools, and workplaces to avoid reinfections that lead to Long COVID? The ridiculously low budgets for the care of those already suffering from Long COVID? The obstacle course to obtain Medicare and Medicaid benefits when you have Long COVID? Patients are misinformed, forced to wander from doctor to doctor, and gaslighted daily by public health institutions, preventing them from becoming aware of their common condition and organizing themselves to force the government to provide a health response commensurate with the epidemic. The state can thus continue to save money at the expense of people living with Long COVID and people with disabilities/chronic illnesses, who have paid the heaviest price since the beginning of the epidemic.
Defining a disease is political. Defining a disease is, above all, the first step toward taking action. The COVID virus continues to circulate actively in France and around the world throughout the year. And with each wave of the epidemic, the number of people falling ill increases. At Winslow Santé Publique, we are well aware that the growing number of people coming to us closely follows the progression of the COVID-19 epidemic. Understanding what Long COVID is means implementing a prevention policy worthy of the name to prevent others from joining us in the disease. It also means steering research in the right direction to find treatments that will truly cure us.
6- OUR PERSPECTIVE ON LONG COVID.
In summary, what is Long COVID for Winslow Santé Publique? It is the combination of all diseases, sequelae, organ damage, and symptoms triggered by the SARS-CoV-2 virus, from the acute infectious phase to the chronic phase of the vascular tropism disease known as COVID. In practice, a person who develops an autoimmune disease (diabetes, lupus, rheumatoid arthritis, Sjögren’s syndrome, etc.), ung or cardiovascular diseases (embolisms, COPD, hypertension, heart attack, fibrosis, stroke, etc.), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), cognitive impairments (brain damage), dysimmunity, or chronic kidney disease due to the SARS-CoV-2 virus, even several months or years after infection, has Long COVID and will continue to have it. Long COVID is all of these things at once, not just a list of symptoms approved by doctors. Long COVID is a chronic, progressive disease, each of whose manifestations can be debilitating and dangerous, and which are often cumulative. It is also a disease for which there is currently no cure and which can lead to death.
We are fighting to ensure that all those affected by the COVID-19 virus have access to the care, treatment, and social rights they are entitled to. Given that nothing is being done by the health authorities to make diagnosis accessible, we also want people to embrace the label “Long COVID” as widely as possible so that they can finally put words to what they are experiencing and what is happening in their bodies since their (re)infection. Like the AIDS activists before us, we will not wait for the health authorities to validate all the manifestations of our illness in order to fit into their definition of Long COVID, because by then we will already be severely disabled or dead. And until objective tests and markers show otherwise, with the frequent chronic persistence of the virus in deep sites of the human body and damage to invisible organs, we will continue to remind people that there is no cure (yet) for Long COVID, even if our symptoms may improve or “disappear.”
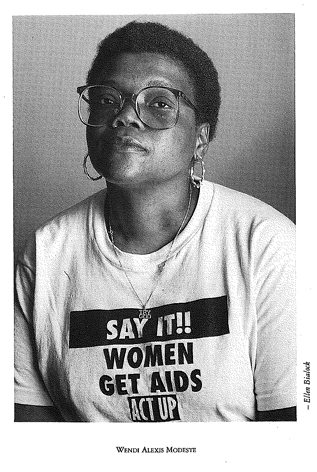
“My name is Wendi Alexis Modeste, I am HIV positive, and I live in New York State. I have had five bouts of recurrent bacterial pneumonia, endocarditis, sepsis, cervical cancer, and pelvic inflammation so severe that I nearly died… And I still don’t fit your damn definition. I want to know one thing: Are you going to keep studying our symptoms until we’re all dead? I’m African American, and my community is changing before my eyes. Ten of my friends died last year, six more this year, and I’m becoming more and more alone. My country is starting to scare me. I want to know: How much longer? »
Translation from french to english (« SIDA, combien de divisions ») of an excerpt from a speech given during the round table discussion on the definition of AIDS at the Amsterdam conference in 1992, Act Up-Paris, 1994: 25
Wendi Alexis Modeste was a black woman living with HIV who was actively involved in the fight against HIV/AIDS as an educator in New York State. Through her advocacy, she contributed, along with others, to updating the definition of AIDS to include symptoms and diseases specific to HIV-positive women. She died of AIDS-related complications in 1994.